AI Chatbot for Insurance Verification & Coverage Guidance
Guide patients through insurance verification, coverage checks, and pre-authorization requirements with an intelligent AI assistant available 24/7.
Trusted by businesses worldwide
Why Insurance Verification Needs Automation
Patients face constant confusion about insurance coverage—whether providers are in-network, what services are covered, pre-authorization requirements, and estimated costs. Staff spend hours on hold with insurance companies while patients wait anxious about coverage and costs. Wonderchat's insurance verification chatbot provides instant guidance on insurance processes—how to check in-network status, what pre-authorization is needed, how to understand coverage documents, and what out-of-pocket costs to expect. Train it on your accepted insurance plans, common verification questions, pre-authorization requirements, and cost estimation processes in 5 minutes. The AI guides patients in 100+ languages, reducing insurance inquiry calls by up to 70%. Healthcare providers gain reduced administrative burden, better-prepared patients, and fewer claim denials from patients who don't understand their coverage. The AI handles routine insurance education while connecting patients needing specific verification, authorization assistance, or insurance disputes to financial coordinators. Transform insurance confusion into clear, supportive patient financial guidance.

Emily
AI Agent
Wonderbot
Welcome to Wonderchat! How can I help you today?
hey i’d like to upgrade to enterprise please
Wonderbot
Sure, please hold on for a second.
Retrieving account details...
Retrieving account details...
Please confirm that you would like to upgrade to Wonderchat Enterprise. Your Visa card ending in 1234 will be charged $480.00 a year.
Cancel
Upgrade
Message...
Easy 5 minute set-up
How Wonderchat Works






Insurance Education Support
Instant Answers to Common Coverage Questions
Deflect up to 70% of routine insurance inquiries about in-network vs. out-of-network coverage, deductibles, co-pays, co-insurance, referral requirements, and how to use insurance benefits—available 24/7 with instant responses.
In-network and out-of-network explanations
Deductible
Referral and authorization requirement information
Insurance Education Support
Instant Answers to Common Coverage Questions
Deflect up to 70% of routine insurance inquiries about in-network vs. out-of-network coverage, deductibles, co-pays, co-insurance, referral requirements, and how to use insurance benefits—available 24/7 with instant responses.
In-network and out-of-network explanations
Deductible
Referral and authorization requirement information
Insurance Education Support
Instant Answers to Common Coverage Questions
Deflect up to 70% of routine insurance inquiries about in-network vs. out-of-network coverage, deductibles, co-pays, co-insurance, referral requirements, and how to use insurance benefits—available 24/7 with instant responses.
In-network and out-of-network explanations
Deductible
Referral and authorization requirement information



Verification Process Guidance
Step-by-Step Insurance Verification Support
Guide patients through insurance verification processes including how to check their coverage online, what information to have ready for verification calls, how to interpret their insurance card, and steps to take if coverage is denied.
How to verify in-network status independently
Understanding insurance card information
Coverage denial next steps and appeal processes
Verification Process Guidance
Step-by-Step Insurance Verification Support
Guide patients through insurance verification processes including how to check their coverage online, what information to have ready for verification calls, how to interpret their insurance card, and steps to take if coverage is denied.
How to verify in-network status independently
Understanding insurance card information
Coverage denial next steps and appeal processes
Verification Process Guidance
Step-by-Step Insurance Verification Support
Guide patients through insurance verification processes including how to check their coverage online, what information to have ready for verification calls, how to interpret their insurance card, and steps to take if coverage is denied.
How to verify in-network status independently
Understanding insurance card information
Coverage denial next steps and appeal processes






Healthcare Billing Standards
HIPAA-Conscious Insurance Guidance
Provide insurance information guidance with HIPAA-conscious standards—answering general insurance process questions without accessing specific patient insurance records, routing account-specific verification to authenticated staff or insurance portals.
HIPAA-conscious insurance information delivery
No PHI or specific account access
Secure routing to verification specialists
Healthcare Billing Standards
HIPAA-Conscious Insurance Guidance
Provide insurance information guidance with HIPAA-conscious standards—answering general insurance process questions without accessing specific patient insurance records, routing account-specific verification to authenticated staff or insurance portals.
HIPAA-conscious insurance information delivery
No PHI or specific account access
Secure routing to verification specialists
Healthcare Billing Standards
HIPAA-Conscious Insurance Guidance
Provide insurance information guidance with HIPAA-conscious standards—answering general insurance process questions without accessing specific patient insurance records, routing account-specific verification to authenticated staff or insurance portals.
HIPAA-conscious insurance information delivery
No PHI or specific account access
Secure routing to verification specialists
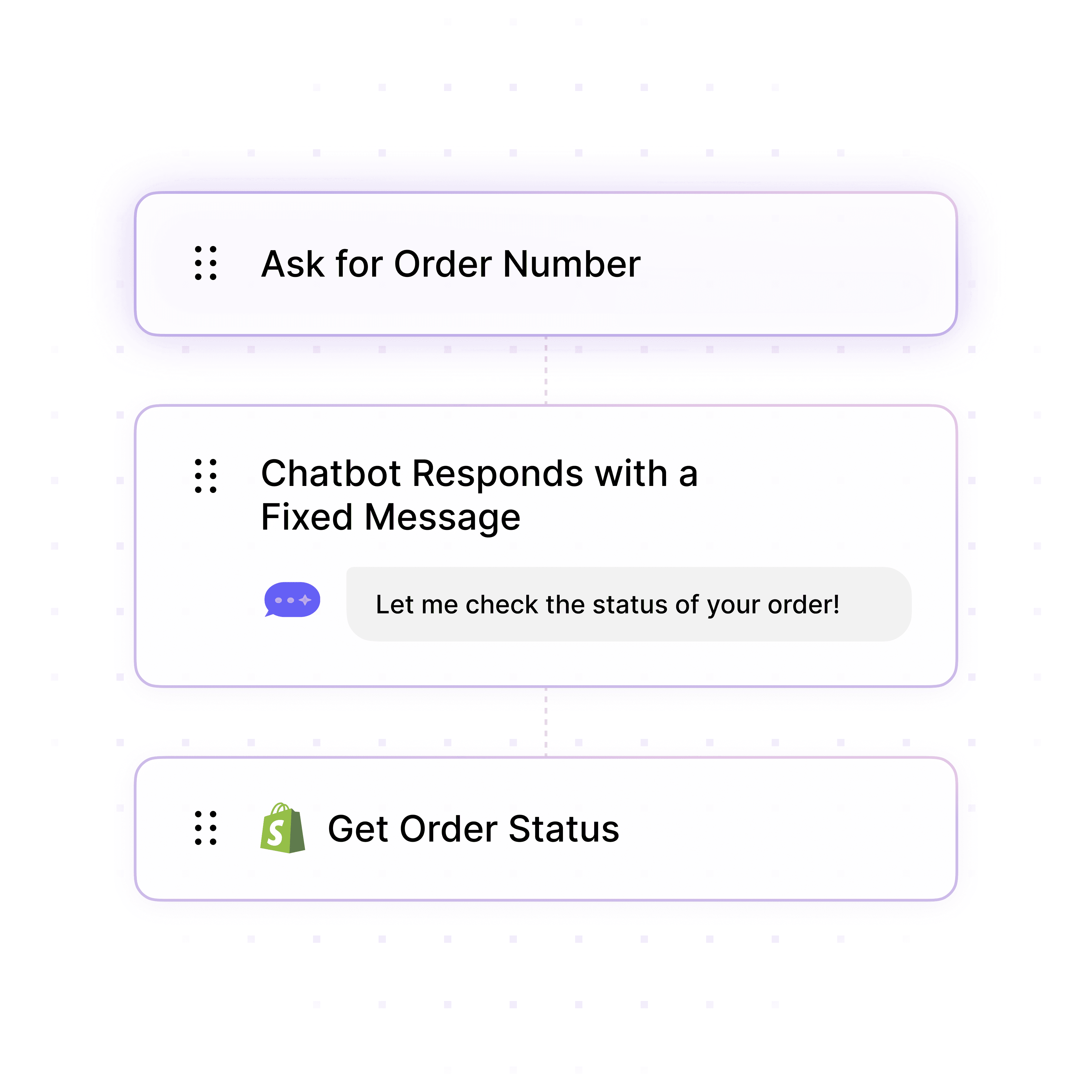
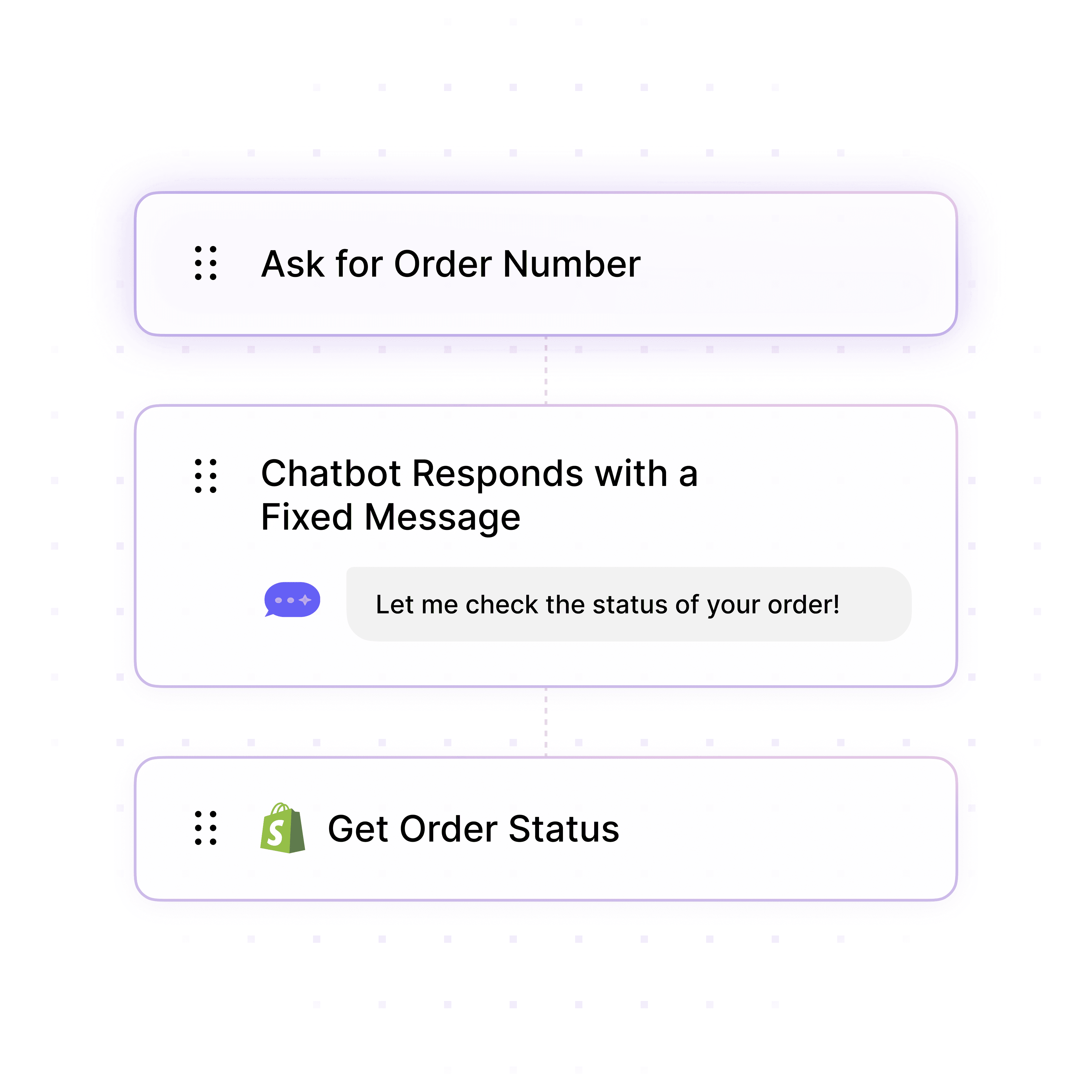
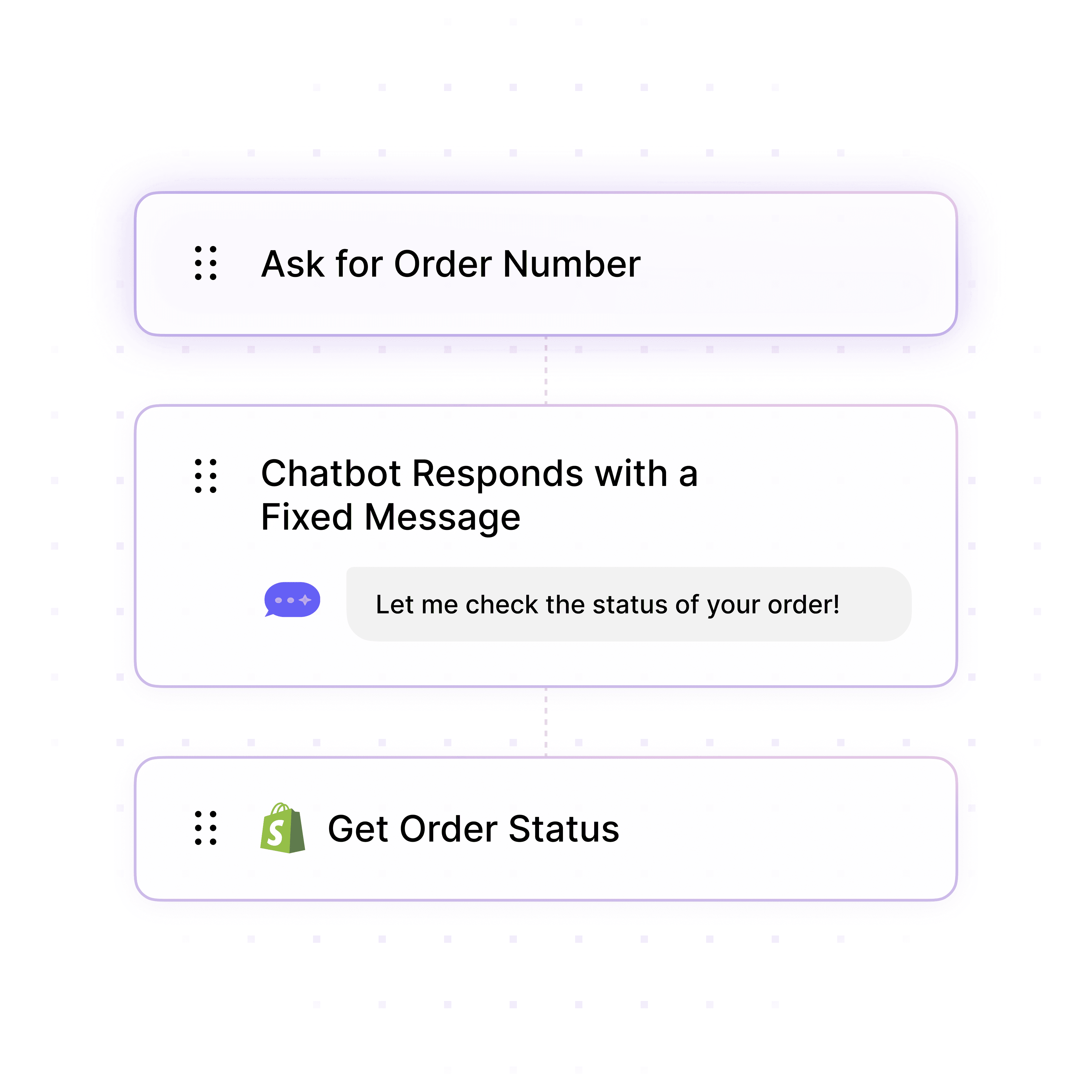
5-minute set up with our native integration
Deploy Your Insurance Verification Chatbot in 5 Minutes
1
Create your AI chatbot – Pick the perfect AI model fit for your support needs.
2
Train AI with Docs, FAQs & Policies – Upload knowledge base files and site links.
3
Customise Workflows & Escalation Rules – AI handles what it can, and escalates what it can’t.
4
Monitor & Optimise with Analytics – See where customers get stuck and fine-tune responses.



Insurance Knowledge Integration
Train on Accepted Plans & Coverage Policies
Upload your accepted insurance plan lists, common insurance terminology explanations, pre-authorization requirement guides, and cost estimation procedures for accurate guidance on coverage questions most common to your patient population.
Accepted insurance plans and network status
Common insurance terms and coverage explanations
Pre-authorization requirements by service type
Insurance Knowledge Integration
Train on Accepted Plans & Coverage Policies
Upload your accepted insurance plan lists, common insurance terminology explanations, pre-authorization requirement guides, and cost estimation procedures for accurate guidance on coverage questions most common to your patient population.
Accepted insurance plans and network status
Common insurance terms and coverage explanations
Pre-authorization requirements by service type
Insurance Knowledge Integration
Train on Accepted Plans & Coverage Policies
Upload your accepted insurance plan lists, common insurance terminology explanations, pre-authorization requirement guides, and cost estimation procedures for accurate guidance on coverage questions most common to your patient population.
Accepted insurance plans and network status
Common insurance terms and coverage explanations
Pre-authorization requirements by service type

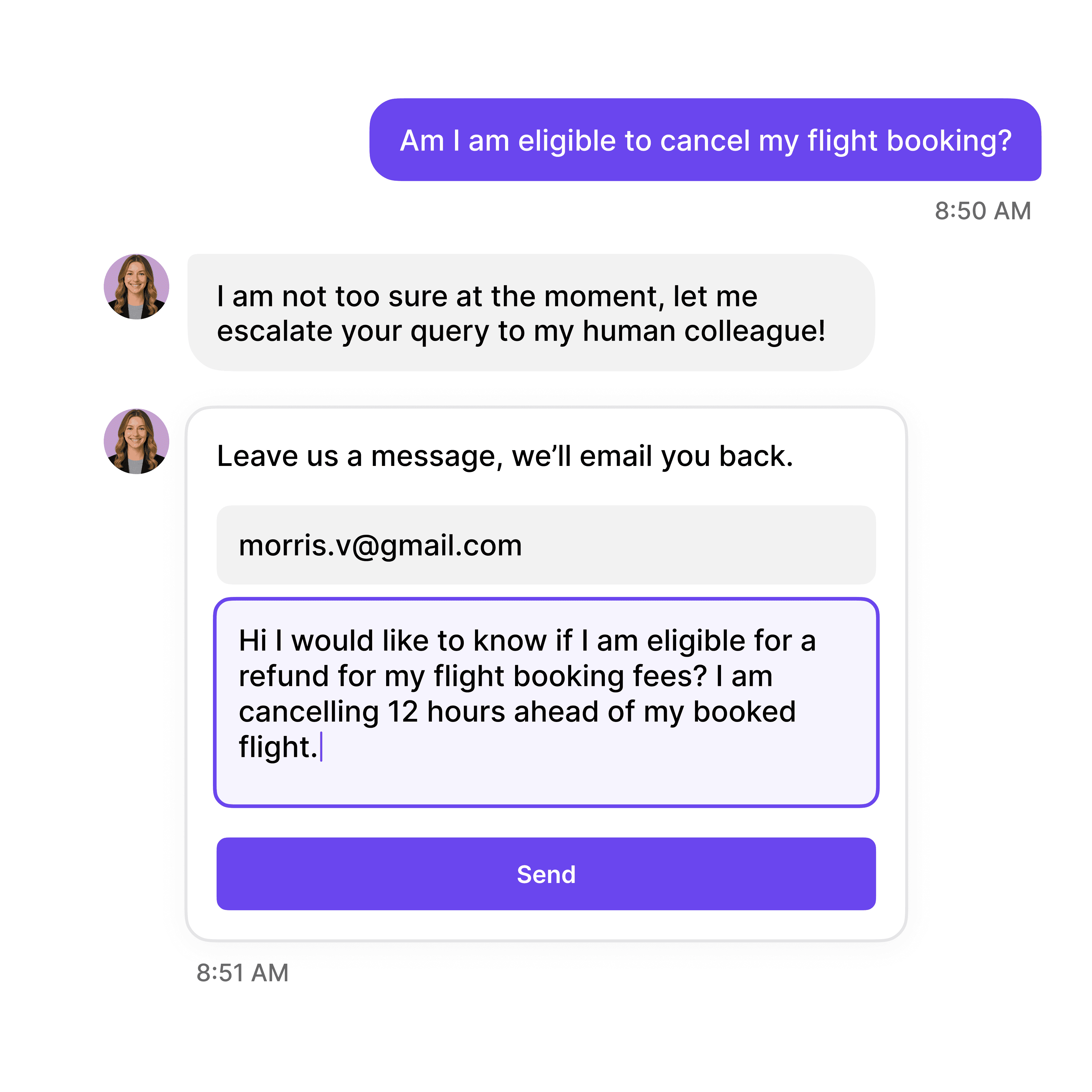


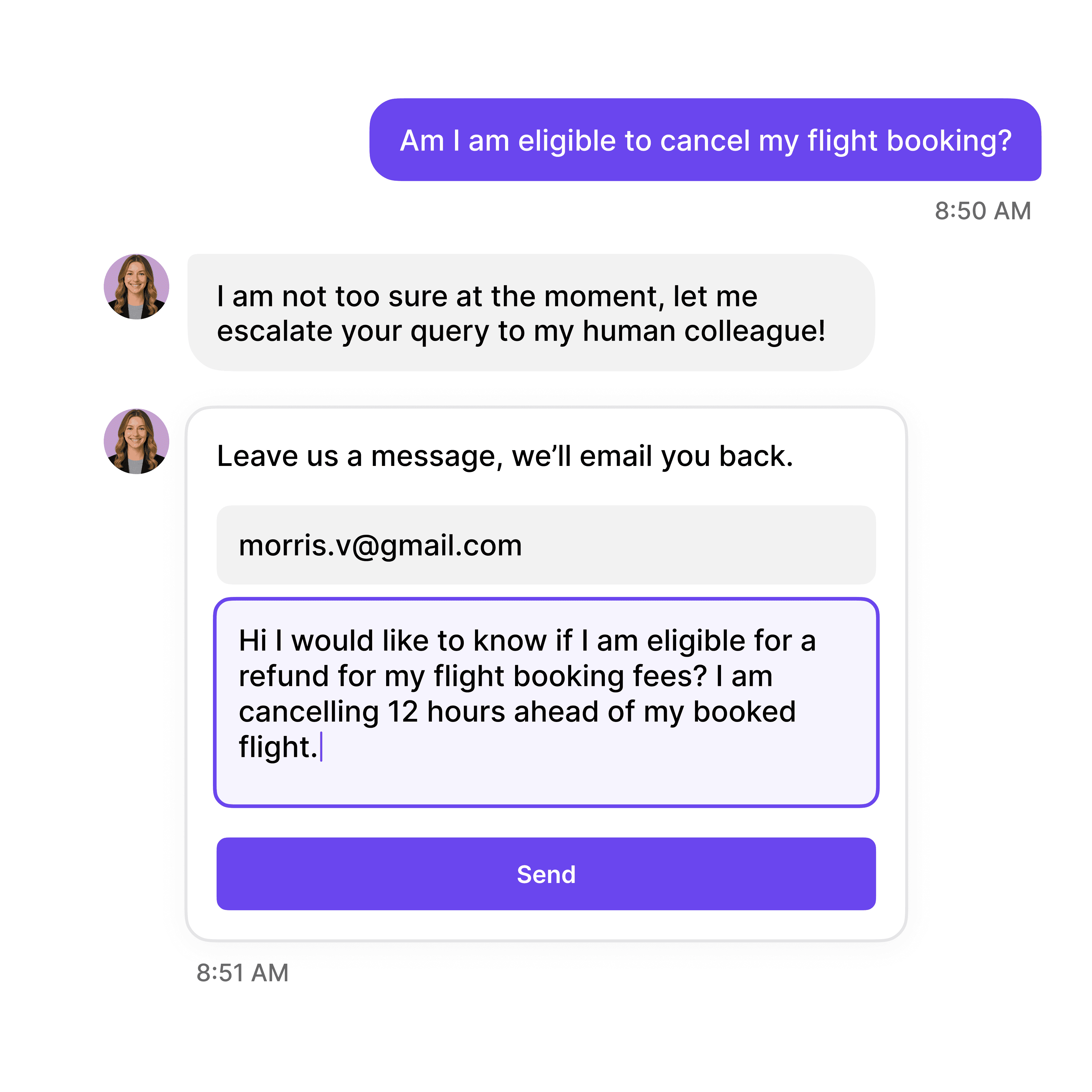


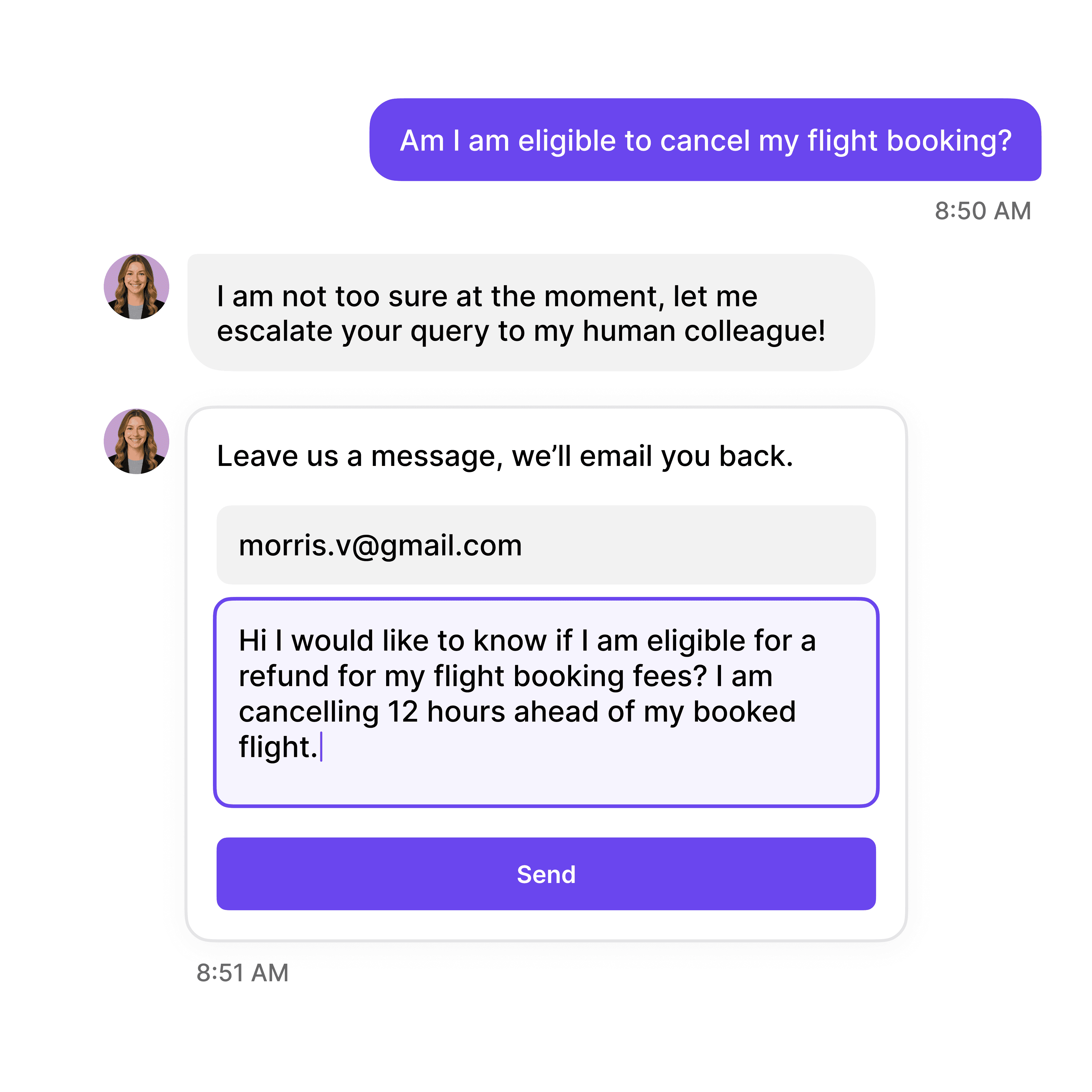

Financial Coordinator Escalation
Connect Coverage Issues to Specialists
Route complex coverage disputes, pre-authorization appeals, insurance denial cases, or patients needing verification assistance to financial coordinators with context on the insurance issue, service needed, and patient's coverage situation.
Complex insurance disputes and claim denials
Pre-authorization appeals and expedited reviews
Patients needing direct verification assistance
Financial Coordinator Escalation
Connect Coverage Issues to Specialists
Route complex coverage disputes, pre-authorization appeals, insurance denial cases, or patients needing verification assistance to financial coordinators with context on the insurance issue, service needed, and patient's coverage situation.
Complex insurance disputes and claim denials
Pre-authorization appeals and expedited reviews
Patients needing direct verification assistance
Financial Coordinator Escalation
Connect Coverage Issues to Specialists
Route complex coverage disputes, pre-authorization appeals, insurance denial cases, or patients needing verification assistance to financial coordinators with context on the insurance issue, service needed, and patient's coverage situation.
Complex insurance disputes and claim denials
Pre-authorization appeals and expedited reviews
Patients needing direct verification assistance
40+ Languages
Starts at $0.02/message
Available 24/7
Start Free Trial
14-day free trial. No credit card required
Testimonials
Businesses with successful customer service start
with Wonderchat

"Wonderchat has made it easier than ever to find the information I need without getting lost in the complexities. It also brings convenience and clarity to my searches."

Josh Levitsky
Global Head of Professional Services, Filewave

“Wonderchat has been a game-changer for bazuba. We’ve seen improved customer satisfaction and a noticeable boost in efficiency. Wonderchat handles our customer queries with precision and speed.

Julien Pflanzl
Web Development Lead, bazuba
“Ever since implementing Wonderchat on our site, I've seen up to a 70% reduction of customer support queries in my inbox.”

Bryce Conway
Founder and CEO, 10xTravel

"Wonderchat has given us the ability to offer real-time answers to our customer’s questions on their terms, pulling from our extensive portfolio of Insurance content. The response has been tremendous."

Ryan Hanley
Founder and President, Rogue Risk LLC

"Wonderchat has made it easier than ever to find the information I need without getting lost in the complexities. It also brings convenience and clarity to my searches."

Josh Levitsky
Global Head of Professional Services, Filewave

“Wonderchat has been a game-changer for bazuba. We’ve seen improved customer satisfaction and a noticeable boost in efficiency. Wonderchat handles our customer queries with precision and speed.

Julien Pflanzl
Web Development Lead, bazuba
“Ever since implementing Wonderchat on our site, I've seen up to a 70% reduction of customer support queries in my inbox.”

Bryce Conway
Founder and CEO, 10xTravel

"Wonderchat has given us the ability to offer real-time answers to our customer’s questions on their terms, pulling from our extensive portfolio of Insurance content. The response has been tremendous."

Ryan Hanley
Founder and President, Rogue Risk LLC

"Wonderchat has made it easier than ever to find the information I need without getting lost in the complexities. It also brings convenience and clarity to my searches."

Josh Levitsky
Global Head of Professional Services, Filewave

“Wonderchat has been a game-changer for bazuba. We’ve seen improved customer satisfaction and a noticeable boost in efficiency. Wonderchat handles our customer queries with precision and speed.

Julien Pflanzl
Web Development Lead, bazuba
“Ever since implementing Wonderchat on our site, I've seen up to a 70% reduction of customer support queries in my inbox.”

Bryce Conway
Founder and CEO, 10xTravel

"Wonderchat has given us the ability to offer real-time answers to our customer’s questions on their terms, pulling from our extensive portfolio of Insurance content. The response has been tremendous."

Ryan Hanley
Founder and President, Rogue Risk LLC

"Wonderchat has made it easier than ever to find the information I need without getting lost in the complexities. It also brings convenience and clarity to my searches."

Josh Levitsky
Global Head of Professional Services, Filewave

“Wonderchat has been a game-changer for bazuba. We’ve seen improved customer satisfaction and a noticeable boost in efficiency. Wonderchat handles our customer queries with precision and speed.

Julien Pflanzl
Web Development Lead, bazuba
“Ever since implementing Wonderchat on our site, I've seen up to a 70% reduction of customer support queries in my inbox.”

Bryce Conway
Founder and CEO, 10xTravel

"Wonderchat has given us the ability to offer real-time answers to our customer’s questions on their terms, pulling from our extensive portfolio of Insurance content. The response has been tremendous."

Ryan Hanley
Founder and President, Rogue Risk LLC

"Wonderchat has made it easier than ever to find the information I need without getting lost in the complexities. It also brings convenience and clarity to my searches."

Josh Levitsky
Global Head of Professional Services, Filewave

“Wonderchat has been a game-changer for bazuba. We’ve seen improved customer satisfaction and a noticeable boost in efficiency. Wonderchat handles our customer queries with precision and speed.

Julien Pflanzl
Web Development Lead, bazuba
“Ever since implementing Wonderchat on our site, I've seen up to a 70% reduction of customer support queries in my inbox.”

Bryce Conway
Founder and CEO, 10xTravel

"Wonderchat has given us the ability to offer real-time answers to our customer’s questions on their terms, pulling from our extensive portfolio of Insurance content. The response has been tremendous."

Ryan Hanley
Founder and President, Rogue Risk LLC

"Wonderchat has made it easier than ever to find the information I need without getting lost in the complexities. It also brings convenience and clarity to my searches."

Josh Levitsky
Global Head of Professional Services, Filewave

“Wonderchat has been a game-changer for bazuba. We’ve seen improved customer satisfaction and a noticeable boost in efficiency. Wonderchat handles our customer queries with precision and speed.

Julien Pflanzl
Web Development Lead, bazuba
“Ever since implementing Wonderchat on our site, I've seen up to a 70% reduction of customer support queries in my inbox.”

Bryce Conway
Founder and CEO, 10xTravel

"Wonderchat has given us the ability to offer real-time answers to our customer’s questions on their terms, pulling from our extensive portfolio of Insurance content. The response has been tremendous."

Ryan Hanley
Founder and President, Rogue Risk LLC

"Wonderchat has made it easier than ever to find the information I need without getting lost in the complexities. It also brings convenience and clarity to my searches."

Josh Levitsky
Global Head of Professional Services, Filewave

“Wonderchat has been a game-changer for bazuba. We’ve seen improved customer satisfaction and a noticeable boost in efficiency. Wonderchat handles our customer queries with precision and speed.

Julien Pflanzl
Web Development Lead, bazuba
“Ever since implementing Wonderchat on our site, I've seen up to a 70% reduction of customer support queries in my inbox.”

Bryce Conway
Founder and CEO, 10xTravel

"Wonderchat has given us the ability to offer real-time answers to our customer’s questions on their terms, pulling from our extensive portfolio of Insurance content. The response has been tremendous."

Ryan Hanley
Founder and President, Rogue Risk LLC

"Wonderchat has made it easier than ever to find the information I need without getting lost in the complexities. It also brings convenience and clarity to my searches."

Josh Levitsky
Global Head of Professional Services, Filewave

“Wonderchat has been a game-changer for bazuba. We’ve seen improved customer satisfaction and a noticeable boost in efficiency. Wonderchat handles our customer queries with precision and speed.

Julien Pflanzl
Web Development Lead, bazuba
“Ever since implementing Wonderchat on our site, I've seen up to a 70% reduction of customer support queries in my inbox.”

Bryce Conway
Founder and CEO, 10xTravel

"Wonderchat has given us the ability to offer real-time answers to our customer’s questions on their terms, pulling from our extensive portfolio of Insurance content. The response has been tremendous."

Ryan Hanley
Founder and President, Rogue Risk LLC

"Wonderchat has made it easier than ever to find the information I need without getting lost in the complexities. It also brings convenience and clarity to my searches."

Josh Levitsky
Global Head of Professional Services, Filewave

“Wonderchat has been a game-changer for bazuba. We’ve seen improved customer satisfaction and a noticeable boost in efficiency. Wonderchat handles our customer queries with precision and speed.

Julien Pflanzl
Web Development Lead, bazuba
“Ever since implementing Wonderchat on our site, I've seen up to a 70% reduction of customer support queries in my inbox.”

Bryce Conway
Founder and CEO, 10xTravel

"Wonderchat has given us the ability to offer real-time answers to our customer’s questions on their terms, pulling from our extensive portfolio of Insurance content. The response has been tremendous."

Ryan Hanley
Founder and President, Rogue Risk LLC

"Wonderchat has made it easier than ever to find the information I need without getting lost in the complexities. It also brings convenience and clarity to my searches."

Josh Levitsky
Global Head of Professional Services, Filewave

“Wonderchat has been a game-changer for bazuba. We’ve seen improved customer satisfaction and a noticeable boost in efficiency. Wonderchat handles our customer queries with precision and speed.

Julien Pflanzl
Web Development Lead, bazuba
“Ever since implementing Wonderchat on our site, I've seen up to a 70% reduction of customer support queries in my inbox.”

Bryce Conway
Founder and CEO, 10xTravel

"Wonderchat has given us the ability to offer real-time answers to our customer’s questions on their terms, pulling from our extensive portfolio of Insurance content. The response has been tremendous."

Ryan Hanley
Founder and President, Rogue Risk LLC

"Wonderchat has made it easier than ever to find the information I need without getting lost in the complexities. It also brings convenience and clarity to my searches."

Josh Levitsky
Global Head of Professional Services, Filewave

“Wonderchat has been a game-changer for bazuba. We’ve seen improved customer satisfaction and a noticeable boost in efficiency. Wonderchat handles our customer queries with precision and speed.

Julien Pflanzl
Web Development Lead, bazuba
“Ever since implementing Wonderchat on our site, I've seen up to a 70% reduction of customer support queries in my inbox.”

Bryce Conway
Founder and CEO, 10xTravel

"Wonderchat has given us the ability to offer real-time answers to our customer’s questions on their terms, pulling from our extensive portfolio of Insurance content. The response has been tremendous."

Ryan Hanley
Founder and President, Rogue Risk LLC

"Wonderchat has made it easier than ever to find the information I need without getting lost in the complexities. It also brings convenience and clarity to my searches."

Josh Levitsky
Global Head of Professional Services, Filewave

“Wonderchat has been a game-changer for bazuba. We’ve seen improved customer satisfaction and a noticeable boost in efficiency. Wonderchat handles our customer queries with precision and speed.

Julien Pflanzl
Web Development Lead, bazuba
“Ever since implementing Wonderchat on our site, I've seen up to a 70% reduction of customer support queries in my inbox.”

Bryce Conway
Founder and CEO, 10xTravel

"Wonderchat has given us the ability to offer real-time answers to our customer’s questions on their terms, pulling from our extensive portfolio of Insurance content. The response has been tremendous."

Ryan Hanley
Founder and President, Rogue Risk LLC

"Wonderchat has made it easier than ever to find the information I need without getting lost in the complexities. It also brings convenience and clarity to my searches."

Josh Levitsky
Global Head of Professional Services, Filewave

“Wonderchat has been a game-changer for bazuba. We’ve seen improved customer satisfaction and a noticeable boost in efficiency. Wonderchat handles our customer queries with precision and speed.

Julien Pflanzl
Web Development Lead, bazuba
“Ever since implementing Wonderchat on our site, I've seen up to a 70% reduction of customer support queries in my inbox.”

Bryce Conway
Founder and CEO, 10xTravel

"Wonderchat has given us the ability to offer real-time answers to our customer’s questions on their terms, pulling from our extensive portfolio of Insurance content. The response has been tremendous."

Ryan Hanley
Founder and President, Rogue Risk LLC

"Wonderchat has made it easier than ever to find the information I need without getting lost in the complexities. It also brings convenience and clarity to my searches."

Josh Levitsky
Global Head of Professional Services, Filewave

“Wonderchat has been a game-changer for bazuba. We’ve seen improved customer satisfaction and a noticeable boost in efficiency. Wonderchat handles our customer queries with precision and speed.

Julien Pflanzl
Web Development Lead, bazuba
“Ever since implementing Wonderchat on our site, I've seen up to a 70% reduction of customer support queries in my inbox.”

Bryce Conway
Founder and CEO, 10xTravel

"Wonderchat has given us the ability to offer real-time answers to our customer’s questions on their terms, pulling from our extensive portfolio of Insurance content. The response has been tremendous."

Ryan Hanley
Founder and President, Rogue Risk LLC

"Wonderchat has made it easier than ever to find the information I need without getting lost in the complexities. It also brings convenience and clarity to my searches."

Josh Levitsky
Global Head of Professional Services, Filewave

“Wonderchat has been a game-changer for bazuba. We’ve seen improved customer satisfaction and a noticeable boost in efficiency. Wonderchat handles our customer queries with precision and speed.

Julien Pflanzl
Web Development Lead, bazuba
“Ever since implementing Wonderchat on our site, I've seen up to a 70% reduction of customer support queries in my inbox.”

Bryce Conway
Founder and CEO, 10xTravel

"Wonderchat has given us the ability to offer real-time answers to our customer’s questions on their terms, pulling from our extensive portfolio of Insurance content. The response has been tremendous."

Ryan Hanley
Founder and President, Rogue Risk LLC

"Wonderchat has made it easier than ever to find the information I need without getting lost in the complexities. It also brings convenience and clarity to my searches."

Josh Levitsky
Global Head of Professional Services, Filewave

“Wonderchat has been a game-changer for bazuba. We’ve seen improved customer satisfaction and a noticeable boost in efficiency. Wonderchat handles our customer queries with precision and speed.

Julien Pflanzl
Web Development Lead, bazuba
“Ever since implementing Wonderchat on our site, I've seen up to a 70% reduction of customer support queries in my inbox.”

Bryce Conway
Founder and CEO, 10xTravel

"Wonderchat has given us the ability to offer real-time answers to our customer’s questions on their terms, pulling from our extensive portfolio of Insurance content. The response has been tremendous."

Ryan Hanley
Founder and President, Rogue Risk LLC
Industry Grade Compliance

Wonderchat is GDPR compliant and AICPA SOC 2 Certified.


FAQ
How does the AI chatbot help patients understand insurance coverage?
Wonderchat explains insurance concepts in plain language—what in-network vs. out-of-network means and why it matters, how deductibles work, the difference between co-pay and co-insurance, when referrals are required, and how pre-authorization affects access to care. This patient education reduces coverage surprises and helps patients make informed decisions about their care.
Can the chatbot confirm if a specific provider or service is in-network?
Wonderchat guides patients to verify in-network status through appropriate channels—your facility's insurance page, insurance company member portals, and direct insurance customer service. For services at your facility, the AI can confirm which insurance plans your organization accepts. For specific patient coverage verification, the AI routes to your financial coordinators or the patient's insurance company.
How does the AI explain pre-authorization requirements?
The chatbot trains on pre-authorization requirements for common services—imaging studies, specialist referrals, procedures, and medications. When patients ask "Do I need pre-authorization for an MRI?" the AI explains the process, typical timelines, and what their provider needs to submit. For urgent or complex authorization situations, the AI escalates to your prior authorization team.
Can the chatbot help patients appeal insurance denials?
Yes, Wonderchat guides patients through the general insurance appeal process—understanding denial reasons, gathering required documentation, typical appeal timelines, and when to request expedited review. The AI provides educational guidance on patient rights in the appeals process while connecting patients with your financial coordinators for personalized appeal assistance.
Does the chatbot support patients with Medicare and Medicaid?
Absolutely. Train Wonderchat on your Medicare and Medicaid acceptance policies, common Medicare Advantage plan questions, Medicaid eligibility basics, and dual-eligible coverage coordination. Patients on government insurance receive accurate guidance on their specific program benefits and how to use their coverage at your facility.
How quickly can healthcare providers deploy the insurance verification chatbot?
Setup takes just 5 minutes. Upload your accepted insurance list, common insurance term explanations, pre-authorization requirement guides, and verification process documentation. Configure HIPAA-conscious guardrails and escalation rules for complex cases, then embed on your website or patient portal for instant 24/7 insurance guidance.
FAQ
How does the AI chatbot help patients understand insurance coverage?
Wonderchat explains insurance concepts in plain language—what in-network vs. out-of-network means and why it matters, how deductibles work, the difference between co-pay and co-insurance, when referrals are required, and how pre-authorization affects access to care. This patient education reduces coverage surprises and helps patients make informed decisions about their care.
Can the chatbot confirm if a specific provider or service is in-network?
Wonderchat guides patients to verify in-network status through appropriate channels—your facility's insurance page, insurance company member portals, and direct insurance customer service. For services at your facility, the AI can confirm which insurance plans your organization accepts. For specific patient coverage verification, the AI routes to your financial coordinators or the patient's insurance company.
How does the AI explain pre-authorization requirements?
The chatbot trains on pre-authorization requirements for common services—imaging studies, specialist referrals, procedures, and medications. When patients ask "Do I need pre-authorization for an MRI?" the AI explains the process, typical timelines, and what their provider needs to submit. For urgent or complex authorization situations, the AI escalates to your prior authorization team.
Can the chatbot help patients appeal insurance denials?
Yes, Wonderchat guides patients through the general insurance appeal process—understanding denial reasons, gathering required documentation, typical appeal timelines, and when to request expedited review. The AI provides educational guidance on patient rights in the appeals process while connecting patients with your financial coordinators for personalized appeal assistance.
Does the chatbot support patients with Medicare and Medicaid?
Absolutely. Train Wonderchat on your Medicare and Medicaid acceptance policies, common Medicare Advantage plan questions, Medicaid eligibility basics, and dual-eligible coverage coordination. Patients on government insurance receive accurate guidance on their specific program benefits and how to use their coverage at your facility.
How quickly can healthcare providers deploy the insurance verification chatbot?
Setup takes just 5 minutes. Upload your accepted insurance list, common insurance term explanations, pre-authorization requirement guides, and verification process documentation. Configure HIPAA-conscious guardrails and escalation rules for complex cases, then embed on your website or patient portal for instant 24/7 insurance guidance.
FAQ
How does the AI chatbot help patients understand insurance coverage?
Wonderchat explains insurance concepts in plain language—what in-network vs. out-of-network means and why it matters, how deductibles work, the difference between co-pay and co-insurance, when referrals are required, and how pre-authorization affects access to care. This patient education reduces coverage surprises and helps patients make informed decisions about their care.
Can the chatbot confirm if a specific provider or service is in-network?
Wonderchat guides patients to verify in-network status through appropriate channels—your facility's insurance page, insurance company member portals, and direct insurance customer service. For services at your facility, the AI can confirm which insurance plans your organization accepts. For specific patient coverage verification, the AI routes to your financial coordinators or the patient's insurance company.
How does the AI explain pre-authorization requirements?
The chatbot trains on pre-authorization requirements for common services—imaging studies, specialist referrals, procedures, and medications. When patients ask "Do I need pre-authorization for an MRI?" the AI explains the process, typical timelines, and what their provider needs to submit. For urgent or complex authorization situations, the AI escalates to your prior authorization team.
Can the chatbot help patients appeal insurance denials?
Yes, Wonderchat guides patients through the general insurance appeal process—understanding denial reasons, gathering required documentation, typical appeal timelines, and when to request expedited review. The AI provides educational guidance on patient rights in the appeals process while connecting patients with your financial coordinators for personalized appeal assistance.
Does the chatbot support patients with Medicare and Medicaid?
Absolutely. Train Wonderchat on your Medicare and Medicaid acceptance policies, common Medicare Advantage plan questions, Medicaid eligibility basics, and dual-eligible coverage coordination. Patients on government insurance receive accurate guidance on their specific program benefits and how to use their coverage at your facility.
How quickly can healthcare providers deploy the insurance verification chatbot?
Setup takes just 5 minutes. Upload your accepted insurance list, common insurance term explanations, pre-authorization requirement guides, and verification process documentation. Configure HIPAA-conscious guardrails and escalation rules for complex cases, then embed on your website or patient portal for instant 24/7 insurance guidance.
40+ Languages
Starts at $0.02/message
Available 24/7
Start Free Trial
14-day free trial. No credit card required
The platform to build AI agents that feel human
Site
© 2025 Wonderchat Private Limited
The platform to build AI agents that feel human
Site
© 2025 Wonderchat Private Limited
The platform to build AI agents that feel human
Site
© 2025 Wonderchat Private Limited







